Abstract
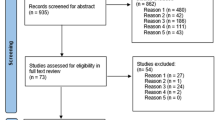
While many may view language barriers in healthcare settings (LBHS) as a simple, practical problem, they present unique challenges to theoretical development and practice implications in healthcare delivery, especially when one considers the implications and impacts of specific contextual factors. By exploring the differences of contextual factors in the US and Japan, this review explores and highlights how such differences may entail different impacts on patients’ quality of care and require different solutions. I conduct narrative review through library database, Google Scholar, and CiNii (a Japanese library database) with multiple search terms, including language barriers, healthcare, medical interpreter, and immigrant. I first present a diagram to show the pathways and process between language barriers and health disparities, using the literature reported in the US. Then, I examined the literature reported in Japan and discuss the needs for re-conceptualizing LBHS. The implications for future research will be discussed.

Similar content being viewed by others
References
Karliner LS, Ma L, Hofmann M, Kerlikowske K. Language barriers, location of care, and delays in follow-up of abnormal mammograms. Med Care. 2012;50:171–8.
Schwei RJ, Del Pozo S, Agger-Gupta N, Alvarado-Little W, Bagchi A, Chen AH, et al. Changes in research on language barriers in health care since 2003: a cross-sectional review study. Int J Nurs Stud. 2015. doi:10.1016/j.ijnurstu.2015.03.001.
Timmins CL. The impact of language barriers on the health care of Latinos in the United States: a review of the literature and guidelines for practice. J Midwifery Women’s Health. 2002;47:80–96.
Jacobs E, Chen AH, Karliner LS, Agger-Gupta N, Mutha S. The need for more research on language barriers in health care: a proposed research agenda. Milbank Q. 2006;84:111–33.
Diamond LC, Schenker Y, Curry L, Bradley EH, Fernandez A. Getting by: underuse of interpreters by resident physicians. JGIM. 2009;24:256–62.
Carrasquillo O, Orav EJ, Brennan TA, Burstin HR. Impact of language barriers on patient satisfaction in an emergency department. JGIM. 1999;14:82–7.
Flores G. Language barriers to health care in the United States. N Engl J Med. 2006;355:229–31.
Divi C, Koss RG, Schmaltz SP, Loeb JM. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007;19:60–7.
Diamond LC, Jacobs EA. Let’s not contribute to disparities: the best methods for teaching clinicians how to overcome language barriers to health care. JGIM. 2010;25:189–93.
Fernandez A, Schillinger D, Warton EM, Adler N, Moffet H, Schenker Y, et al. Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE). JGIM. 2011;26:170–6.
Sentell T, Braun KL, Davis J, Davis T. Colorectal cancer screening: low health literacy and limited English proficiency among Asians and Whites in California. J Health Commun. 2013;18:242–55.
Butow P, Bell M, Goldstein D, Sze M, Aldridge L, Abdo S, et al. Grappling with cultural differences; communication between oncologists and immigrant cancer patients with and without interpreters. Patient Educ Counsel. 2011;84:398–405.
Barber BR. Jihad vs. McWorld. New York: The Random House Publishing Group; 1995.
Hofstede G. Culture’s consequences: international differences in work-related values. Beverly Hills: Sage; 1980.
Akabayashi A, Fetters MD, Elwyn TS. Family consent, communication, and advance directives for cancer disclosure: a Japanese case and discussion. J Med Ethics. 1999;25:296–301.
De Jong G, Steinmetz M. Receptivity attitudes and the occupational attainment of male and female immigrant workers. Popul Res Policy Rev. 2004;23:91–116.
Prins E, Toso BW. Receptivity toward immigrants in rural Pennsylvania: perceptions of adult English as second language providers. Rural Sociol. 2012;77:435–61.
Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med. 2006;5:101–17.
Baumeister RF, Leary MR. Writing narrative literature reviews. Rev Gener Psychol. 1997;1:311–20.
Gregg J, Saha S. Communicative competence: a framework for understanding language barriers in health care. JGIM. 2007;22:368–70.
Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Educ Couns. 2009;74:295–301.
Campbell SM, Roland MO, Buetow SA. Defining quality of care. Soc Sci Med. 2000;51:1611–25.
Ndiaye K, Krieger JL, Warren JR, Hecht ML. Communication and health disparity. In: Thompson TL, Parrott R, Nussbaum JF, editors. The Routledge handbook of health communication. 2nd ed. New York, NY: Routledge; 2011. p. 469–81.
Kleinman A. Patients and healers in the context of culture: an exploration of the borderland between anthropology, medicine, and psychiatry. London: University of California Press; 1980.
Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31:S19–26.
Institute of Medicine. Unequal treatment: what healthcare providers need to know about racial and ethnic disparities in healthcare. Institute of Medicine; 2002.
Piette JD, Bibbins-Domingo K, Schillinger D. Health care discrimination, processes of care, and diabetes patients’ health status. Patient Educ Couns. 2006;60:41–8.
Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20–47.
Bradac JJ, Giles H. Language and social psychology: conceptual niceties, complexities, curiosities, monstrosities, and how it all works. In: Fitch KL, Sanders RE, editors. Handbook of language and social interaction. Mahwah, NJ: Lawrence Erlbaum Associates; 2005. p. 201–30.
Stuber J, Meyer I, Link B. Stigma, prejudice, discrimination and health. Soc Sci Med. 2008;67:351–7.
Lambert WE, Hodgson RC, Gardner RC, Fillenbaum S. Evaluational reactions to spoken languages. J Abnorm Soc Psychol. 1964;60:44–51.
Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: a biopsychosocial model. Am Psychol. 1999;54:805.
Goffman E. Stigma: notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice-Hall; 1963.
Thomas SB, Fine MJ, Ibrahim SA. Health disparities: the importance of culture and health communication. Am J Public Health. 2004;94:2050.
Youdelman MK. The medical tongue: U.S. laws and policies on language access. Health Aff. 2008;27:424–33.
DeCamp LR, Kieffer E, Zickafoose JS, DeMonner S, Valbuena F, Davis MM, et al. The voices of limited English proficiency Latina mothers on pediatric primary care: lessons for the medical home. Matern Child Health J. 2013;17:95–109.
Paasche-Orlow MK, Wilson EAH, McCormack L. The evolving field of health literacy research. J Health Commun. 2010;15:5–8.
Kuo DZ, O’Connor KG, Flores G, Minkovitz CS. Pediatricians’ use of language services for families with limited English proficiency. Pediatrics. 2007;119:e920–7.
Jang M, Lee E, Woo K. Income, language, and citizenship status: factors affecting the health care access and utilization of Chinese Americans. Health Soc Work. 1998;23:136–45.
Feinberg E, Swartz K, Zaslavsky A, Gardner J, Walker D. Language proficiency and the enrollment of Medicaid-eligible children in publicly funded health insurance programs. Matern Child Health J. 2002;6:5–18.
Conrad P, Barker KK. The social construction of illness: key insights and policy implications. J Health Soc Behav. 2010;51:S67–79.
Ngo-Metzger Q, Sorkin DH, Phillips RS. Healthcare experiences of limited english-proficient asian american patients: a cross-sectional mail survey. Patient. 2009;2:113–20.
Woloshin S, Bickell NA, Schwartz LM, Gany F, Welch HG. Language barriers in medicine in the United States. JAMA. 1995;273:724–8.
Wilson E, Chen AH, Grumbach K, Wang F, Fernandez A. Effects of limited English proficiency and physician language on health care comprehension. JGIM. 2005;20:800–6.
John-Baptiste A, Naglie G, Tomlinson G, Alibhai SMH, Etchells E, Cheung A, et al. The effect of English language proficiency on length of stay and in-hospital mortality. JGIM. 2004;19:221–8.
Kravitz RL, Helms LJ, Azari R, Antonius D, Melnikow J. Comparing the use of physician time and health care resources among patients speaking English, Spanish, and Russian. Med Care. 2000;38:728–38.
Bernstein J, Bernstein E, Dave A, Hardt E, James T, Linden J, et al. Trained medical interpreters in the emergency department: effects on services, subsequent charges, and follow-up. J Immigr Health. 2002;4:171–6.
Sarver J, Baker D. Effect of language barriers on follow-up appointments after an emergency department visit. JGIM. 2000;15:256–64.
Goldenberg M. Defining, “quality of care” persuasively. Theor Med Bioeth. 2012;33:243–61.
Mutchler J, Bacigalupe G, Coppin A, Gottlieb A. Language barriers surrounding medication use among older Latinos. J Cross-Cult Gerontol. 2007;22:101–14.
Fernandez A, Schillinger D, Grumbach K, Rosenthal A, Stewart A, Wang F, et al. Physician language ability and cultural competence. JGIM. 2004;19:167–74.
Diamond LC, Reuland DS. Describing physician language fluency: deconstructing medical Spanish. JAMA. 2009;301:426–8.
Andrulis DP, Brach C. Integrating literacy, culture, and language to improve health care quality for diverse populations. Am J Health Behav. 2007;31:s122–33.
Messias DKH, McDowell L, Estrada RD. Language interpreting as social justice work: perspectives of formal and informal healthcare interpreters. ANS Adv Nurs Sci. 2009;32:128–43.
Baker DW, Parker RM, Williams MV, Coates WC, Pitkin K. Use and effectiveness of interpreters in an emergency department. JAMA. 1996;275:783–8.
Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42:727–54.
Flores G, Abreu M, Barone CP, Bachur R, Lin H. Errors of medical interpretation and their potential clinical consequences: a comparison of professional versus ad hoc versus no interpreters. Ann Emerg Med. 2012;60:545–53.
Drennan G, Swartz L. The paradoxical use of interpreting in psychiatry. Soc Sci Med. 2002;54:1853–66.
Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62:255–99.
Fagan MJ, Diaz JA, Reinert SE, Sciamanna CN, Fagan DM. Impact of interpretation method on clinic visit length. JGIM. 2003;18:634–8.
Abbe M, Simon C, Angiolillo A, Ruccione K, Kodish ED. A survey of language barriers from the perspective of pediatric oncologists, interpreters, and parents. Pediatr Blood Cancer. 2006;47:819–24.
Ginde A, Clark S, Camargo C Jr. Language barriers among patients in Boston emergency departments: use of medical interpreters after passage of interpreter legislation. J Immigr Minor Health. 2009;11:527–30.
Jacobs E. A better measure of patients’ need for interpreter services. JGIM. 2008;23:1724–5.
Derose KP, Hays RD, McCaffrey DF, Baker DW. Does physician gender affect satisfaction of men and women visiting the emergency department? JGIM. 2001;16:218–26.
O’Leary SCB, Federico S, Hampers LC. The truth about language barriers: one residency program’s experience. Pediatrics. 2003;111:569.
Yawman D, McIntosh S, Fernandez D, Auinger P, Allan M, Weitzman M. The use of Spanish by medical students and residents at one university hospital. Acad Med. 2006;81:468–73.
Schenker Y, Wang F, Selig SJ, Ng R, Fernandez A. The impact of language barriers on documentation of informed consent at a hospital with on-site interpreter services. JGIM. 2007;22:294–9.
Andres E, Wynia M, Regenstein M, Maul L. Should I call an interpreter? How do physicians with second language skills decide? J Health Care Poor Underserved. 2013;24:525–39.
Hsieh E. Not just “getting by”: factors influencing providers’ choice of interpreters. JGIM. 2015;30:75–82.
Rosenberg E, Seller R, Leanza Y. Through interpreters’ eyes: comparing roles of professional and family interpreters. Patient Educ Couns. 2008;70:87–93.
Karliner LS, Auerbach A, Napoles A, Schillinger D, Nickleach D, Perez-Stable EJ. Language barriers and understanding of hospital discharge instructions. Med Care. 2012;50:283–9.
Leyva M, Sharif I, Ozuah PO. Health literacy among Spanish-speaking Latino parents with limited English proficiency. Ambul Pediatr. 2005;5:56–9.
Wilson E, Chen AH, Grumbach K, Wang F, Fernandez A. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20:800–6.
Xu KT, Rojas-Fernandez CH. Ancillary community pharmacy services provided to older people in a largely rural and ethnically diverse region: a survey of consumers in West Texas. J Rural Health. 2003;19:79–86.
Westberg SM, Sorensen TD. Pharmacy-related health disparities experienced by non-English-speaking patients: impact of pharmaceutical care. J Am Pharm Assoc. 2005;45:48–54.
Sleath B. Pharmacists’ experiences in and perceptions toward serving the needs of Spanish-speaking patients in North Carolina community pharmacies. J Pharm Teach. 2002;9:77–91.
Muzyk AJ, Muzyk TL, Barnett CW. Counseling Spanish-speaking patients: Atlanta pharmacists’ cultural sensitivity, use of language-assistance services, and attitudes. J Am Pharm Assoc. 2003;44:366–74.
Ohtsuki S. Japanese views over the increase in foreigners: using JGSS-2003 data [Japanese]. 社会学論考. 2007;28:1–25.
Terasawa T. 英語以外の異言語に対する「日本人」の態度の社会統計的分析 [Japanese]. 東京大学大学院総合文化研究科言語情報科学専攻. 2014;3:91–107.
Takahashi M. The role of interpreters: from the perspectives of community interpreters [Japanese]. Tokyo University of Foreign Studies: Center for Multilingual Multicultural Education and Research; 2009, p. 50–62.
Iida N. The present condition and problems of community interpreters involved in the support system for returnees from China: a study of interpreter roles [Japanese]. 立命館人間科学研究. 2010;21:75–88.
Okubo T. The national health insurance program and illegal immigrants [Japanese]. 社会研論集. 2004;4:141–53.
Ueda A, Ogihara A, Yamaji M, Mitani H. Fact-finding survey on medical information for foreign residents on the web sites of local governments in Japan [Japanese]. Bull Soc Med. 2011;29:63–71.
Kawauchi K. Problems of medical interpreters in Japan [Japanese]. J Aomori Univ Health Welf. 2011;12:33–40.
Wakimoto T, Chisaki M, Uchida K. The perspectives of medical treatment provided to foreign individuals: the role of medical interpretors [Japanese]. J Pediatr Pract. 2013;76:971–5.
Hasegawa T, Takeda C, Tsukida K, Shirakawa K. A study of nursing care for foreigners in Japan [Japanese]. Fukui Med Res J. 2002;3:49–55.
Ministry of Justice. Statistics of foreign residents. 2014.
Maeno M, Enomoto N, Maeno R, Tamaki Y, Tanakamaru H, Fujihara A. The problem of foreign language translation and supporting for foreigners in clinics accepting foreigners [Japanese] 研究紀要. 2010:13–26.
Nakagawa K, Takuwa N. A study on the present status and prospect on medical care for foreign patients in Ishikawa Prefecture: based on a questionnaire survey for registered medical institutes for foreigners [Japanese]. Ishikawa J Nursing. 2012;9:23–32.
Non Profit Organization: Advanced Medical Promotion Organization. Large hospitals in Tokyo: thirty percent indicated the difficulty to accept patients with language barriers [Japanese]. 特定非営利活動団体 先端医療推進機構; 2013.
Park J-G. Foreign language edition home page: Chica city administration home page [Japanese]. 東京情報大学研究論集. 2007;10:11–20.
Abe Y. Necessity for community interpreters to manage mental illness [Japanese]. Tokyo University of Foreign Studies: Center for Multilingual Multicultural Education and Research. 2013, p. 105–113.
Arai K, Sasaki A, Sato C. 外国人妊産婦に対する産科病棟の対応 [Japanese]. 助産雑誌. 2006;60:355–60.
Miyabe M, Yoshino T, Shigeno A. Development of a multilngual medical reception support system based on parallel texts for foreign patients [Japanese]. 電子情報通信学会論文誌. 2009;J92-D:708–18.
Foundation of Global Health Care. Certification for bilingual medical staff (CBMS). 2014.
Iida N. The present condition and problems of medical interpreters for the foreigners living in Japan and visiting Japan [Japanese]. 立命館人間科学研究. 2011;23:47–57.
Usui S. Foreign residents’ experiences in the Japanese health care system and evaluation of their satisfaction [Japanese]: Tokyo Metropolitan University; 2013.
Schenker Y, Karter AJ, Schillinger D, Warton EM, Adler NE, Moffet HH, et al. The impact of limited English proficiency and physician language concordance on reports of clinical interactions among patients with diabetes: The DISTANCE study. Patient Educ Couns. 2010;81:222–8.
Kim KI, Park H-J, Suzuki N. Reward allocations in the United States, Japan, and Korea: a comparison of individualistic and collectivistic cultures. Acad Manag J. 1990;33:188–98.
Brown P, Levinson SC. Politeness: some universals in language usage. Cambridge: Cambridge University Press; 1987.
Akechi T, Miyashita M, Morita T, Okuyama T, Sakamoto M, Sagawa R, et al. Good death in elderly adults with cancer in Japan based on perspectives of the general population. J Am Geriatr Soc. 2012;60:271–6.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Terui, S. Conceptualizing the Pathways and Processes Between Language Barriers and Health Disparities: Review, Synthesis, and Extension. J Immigrant Minority Health 19, 215–224 (2017). https://doi.org/10.1007/s10903-015-0322-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-015-0322-x