Abstract
Objectives
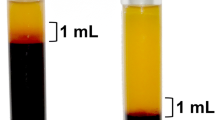
Platelet-rich fibrin (PRF) has been utilized in regenerative dentistry as a supra-physiological concentrate of autologous growth factors capable of stimulating tissue regeneration. Due to the variability in the macroscopic morphology/size of PRF membranes observed between patients, we were interested in studying the effects of patient age, gender, and time between blood draw and the start of centrifugation on the size outcomes of PRF membranes. Despite PRF therapy being increasingly more popular in private practice, to date, no study has investigated the effects of the delay between blood draw and the start of centrifugation in a clinical setting.
Materials and methods
A total of 60 patients enrolled in this study were divided into 6 groups of 10 patients each, including male and female patients categorized into age groups 21–40, 41–60, and 61–80 years. From each patient, a total of five PRF membranes were fabricated from 10-mL tubes following centrifugation starting after 0, 30, 60, 90, and 120 s. In total, 300 PRF membranes were produced in this study to investigate the effects of patient age, gender, and time on the size outcomes of PRF membranes.
Results
A longer delay by the clinician before starting centrifugation following blood draw led to a smaller final size of PRF membranes. At 90 s following blood draw, a significant (13%) reduction in PRF membrane size was observed. After 120 s, a significant (23%) reduction was observed. Additionally, female patients had on average 17% larger membranes compared to men (p < 0.05, 300 samples). Lastly, the size outcomes of the PRF membranes was largest in patients aged 61–80, followed by those aged 41–60 and 21–40. However, no statistically significant differences in PRF membrane sizes were reported between age groups.
Conclusions
The time at which a centrifugation procedure begins following blood draw is critical to optimize the size outcomes of PRF membranes. In general, approximately 15 s is required per tube to harvest 9–10 cc of blood. Therefore, a 60- to 90-s interval between blood draw and the start of centrifugation should be a parameter that is respected by clinicians to avoid significant changes in the macroscopic morphology/size of fabricated PRF membranes. Furthermore, females and older patients produced larger membranes, likely due to lower red blood cell counts derived from their peripheral blood.
Clinical relevance
The findings from the present study demonstrate that on average, a clinician has approximately 60–90 s between blood draw and the start of the centrifugation cycle to produce standard-sized PRF membranes. Shortly thereafter, a significant reduction in size is observed. Additionally, females and older patients were found to produce larger PRF membranes. Centrifugation protocols may therefore be adapted accordingly.





Similar content being viewed by others
References
Miron RJ, Zucchelli G, Pikos MA, Salama M, Lee S, Guillemette V, Fujioka-Kobayashi M, Bishara M, Zhang Y, Wang HL, Chandad F, Nacopoulos C, Simonpieri A, Aalam AA, Felice P, Sammartino G, Ghanaati S, Hernandez MA, Choukroun J (2017) Use of platelet-rich fibrin in regenerative dentistry: a systematic review. Clin Oral Investig 21:1913–1927. https://doi.org/10.1007/s00784-017-2133-z
Chow TW, McIntire LV, Peterson DM (1983) Importance of plasma fibronectin in determining PFP and PRP clot mechanical properties. Thromb Res 29:243–248
Delaini F, Poggi A, Donati MB (1982) Enhanced affinity for arachidonic acid in platelet-rich plasma from rats with Adriamycin-induced nephrotic syndrome. Thromb Haemost 48:260–262
Marx RE (2004) Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg 62:489–496
Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR (1998) Platelet-rich plasma: growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol oral Radiol Endod 85:638–646
Cai YZ, Zhang C, Lin XJ (2015) Efficacy of platelet-rich plasma in arthroscopic repair of full-thickness rotator cuff tears: a meta-analysis. J Shoulder Elb Surg 24:1852–1859. https://doi.org/10.1016/j.jse.2015.07.035
Meheux CJ, McCulloch PC, Lintner DM, Varner KE, Harris JD (2016) Efficacy of intra-articular platelet-rich plasma injections in knee osteoarthritis: a systematic review. Arthroscopy 32:495–505. https://doi.org/10.1016/j.arthro.2015.08.005
Singh B, Goldberg LJ (2016) Autologous platelet-rich plasma for the treatment of pattern hair loss. Am J Clin Dermatol 17:359–367. https://doi.org/10.1007/s40257-016-0196-2
Anfossi G, Trovati M, Mularoni E, Massucco P, Calcamuggi G, Emanuelli G (1989) Influence of propranolol on platelet aggregation and thromboxane B2 production from platelet-rich plasma and whole blood. Prostaglandins Leukot Essent Fat Acids 36:1–7
Fijnheer R, Pietersz RN, de Korte D, Gouwerok CW, Dekker WJ, Reesink HW, Roos D (1990) Platelet activation during preparation of platelet concentrates: a comparison of the platelet-rich plasma and the buffy coat methods. Transfusion 30:634–638
Kobayashi E, Fluckiger L, Fujioka-Kobayashi M, Sawada K, Sculean A, Schaller B, Miron RJ (2016) Comparative release of growth factors from PRP, PRF, and advanced-PRF. Clin Oral Investig 20:2353–2360. https://doi.org/10.1007/s00784-016-1719-1
Fujioka-Kobayashi M, Miron RJ, Hernandez M, Kandalam U, Zhang Y, Choukroun J (2017) Optimized platelet-rich fibrin with the low-speed concept: growth factor release, biocompatibility, and cellular response. J Periodontol 88:112–121. https://doi.org/10.1902/jop.2016.160443
Kubesch A, Barbeck M, Al-Maawi S, Orlowska A, Booms PF, Sader RA, Miron RJ, Kirkpatrick CJ, Choukroun J, Ghanaati S (2018) A low-speed centrifugation concept leads to cell accumulation and vascularization of solid platelet-rich fibrin: an experimental study in vivo. Platelets:1–12. https://doi.org/10.1080/09537104.2018.1445835
Wend S, Kubesch A, Orlowska A, Al-Maawi S, Zender N, Dias A, Miron RJ, Sader R, Booms P, Kirkpatrick CJ, Choukroun J, Ghanaati S (2017) Reduction of the relative centrifugal force influences cell number and growth factor release within injectable PRF-based matrices. J Mater Sci Mater Med 28:188. https://doi.org/10.1007/s10856-017-5992-6
Miron RJ, Fujioka-Kobayashi M, Hernandez M, Kandalam U, Zhang Y, Ghanaati S, Choukroun J (2017) Injectable platelet rich fibrin (i-PRF): opportunities in regenerative dentistry? Clin Oral Investig 21:2619–2627. https://doi.org/10.1007/s00784-017-2063-9
Nunes CR, Roedersheimer M, Simske S, Luttges M (1995) Effect of microgravity, temperature, and concentration on fibrin and collagen assembly. Microgravity Sci Technol 8:125–130
Dohan Ehrenfest DM, Del Corso M, Diss A, Mouhyi J, Charrier J-B (2010) Three-dimensional architecture and cell composition of a Choukroun’s platelet-rich fibrin clot and membrane. J Periodontol 81:546–555
Yajamanya SR, Chatterjee A, Babu CN, Karunanithi D (2016) Fibrin network pattern changes of platelet-rich fibrin in young versus old age group of individuals: a cell block cytology study. J Indian Soc Periodontol 20:151
Miron RJ, Choukroun J (2017) Platelet rich fibrin in regenerative dentistry: biological background and clinical indications. John Wiley & Sons
Sammartino G, Dohan Ehrenfest DM, Carile F, Tia M, Bucci P (2011) Prevention of hemorrhagic complications after dental extractions into open heart surgery patients under anticoagulant therapy: the use of leukocyte- and platelet-rich fibrin. J Oral Implantol 37:681–690. https://doi.org/10.1563/aaid-joi-d-11-00001
Hoaglin DR, Lines GK (2013) Prevention of localized osteitis in mandibular third-molar sites using platelet-rich fibrin. Int J Dent 2013:875380. https://doi.org/10.1155/2013/875380
Suttapreyasri S, Leepong N (2013) Influence of platelet-rich fibrin on alveolar ridge preservation. J Craniofac Surg 24:1088–1094. https://doi.org/10.1097/SCS.0b013e31828b6dc3
Yelamali T, Saikrishna D (2015) Role of platelet rich fibrin and platelet rich plasma in wound healing of extracted third molar sockets: a comparative study. J Maxillofac Oral Surg 14:410–416. https://doi.org/10.1007/s12663-014-0638-4
Anilkumar K, Geetha A, Umasudhakar RT, Vijayalakshmi R, Pameela E (2009) Platelet-rich-fibrin: a novel root coverage approach. J Indian Soc Periodontol 13:50–54. https://doi.org/10.4103/0972-124x.51897
Jankovic S, Aleksic Z, Klokkevold P, Lekovic V, Dimitrijevic B, Kenney EB, Camargo P (2012) Use of platelet-rich fibrin membrane following treatment of gingival recession: a randomized clinical trial. Int J Periodontics Restorative Dent 32:e41–e50
Eren G, Tervahartiala T, Sorsa T, Atilla G (2015) Cytokine (interleukin-1beta) and MMP levels in gingival crevicular fluid after use of platelet-rich fibrin or connective tissue graft in the treatment of localized gingival recessions. J Periodontal Res 51:481–488. https://doi.org/10.1111/jre.12325
Jain V, Triveni MG, Kumar AB, Mehta DS (2012) Role of platelet-rich-fibrin in enhancing palatal wound healing after free graft. Contemp Clin Dent 3:S240–S243. https://doi.org/10.4103/0976-237x.101105
Kulkarni MR, Thomas BS, Varghese JM, Bhat GS (2014) Platelet-rich fibrin as an adjunct to palatal wound healing after harvesting a free gingival graft: a case series. J Indian Soc Periodontol 18:399–402. https://doi.org/10.4103/0972-124x.134591
Femminella B, Iaconi MC, Di Tullio M, Romano L, Sinjari B, D’Arcangelo C, De Ninis P, Paolantonio M (2016) Clinical comparison of platelet-rich fibrin and a gelatin sponge in the management of palatal wounds after epithelialized free gingival graft harvest: a randomized clinical trial. J Periodontol 87:103–113. https://doi.org/10.1902/jop.2015.150198
Ajwani H, Shetty S, Gopalakrishnan D, Kathariya R, Kulloli A, Dolas RS, Pradeep AR (2015) Comparative evaluation of platelet-rich fibrin biomaterial and open flap debridement in the treatment of two and three wall intrabony defects. J Int Oral Health 7:32–37
di Lauro AE, Abbate D, Dell’Angelo B, Iannaccone GA, Scotto F, Sammartino G (2015) Soft tissue regeneration using leukocyte-platelet rich fibrin after exeresis of hyperplastic gingival lesions: two case reports. J Med Case Rep 9:252. https://doi.org/10.1186/s13256-015-0714-5
Miron RJ, Fujioka-Kobayashi M, Bishara M, Zhang Y, Hernandez M, Choukroun J (2016) Platelet-rich fibrin and soft tissue wound healing: a systematic review. Tissue Eng B Rev 23:83–99. https://doi.org/10.1089/ten.TEB.2016.0233
Zeng SM, Yankowitz J, Widness JA, Strauss RG (2001) Etiology of differences in hematocrit between males and females: sequence-based polymorphisms in erythropoietin and its receptor. J Gend Specif Med 4:35–40
Billett HH (1990) Hemoglobin and hematocrit
Ghanaati S, Booms P, Orlowska A, Kubesch A, Lorenz J, Rutkowski J, Landes C, Sader R, Kirkpatrick C, Choukroun J (2014) Advanced platelet-rich fibrin: a new concept for cell-based tissue engineering by means of inflammatory cells. J Oral Implant 40:679–689. https://doi.org/10.1563/aaid-joi-D-14-00138
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
No ethical approval was required for this study, as human samples were not identified.
Informed consent
For this type of study, informed consent was provided prior to blood draw to conduct the outlined experiments.
Rights and permissions
About this article
Cite this article
Miron, R.J., Dham, A., Dham, U. et al. The effect of age, gender, and time between blood draw and start of centrifugation on the size outcomes of platelet-rich fibrin (PRF) membranes. Clin Oral Invest 23, 2179–2185 (2019). https://doi.org/10.1007/s00784-018-2673-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2673-x