The entrance exam to medical school consists of a six-hour fusillade of hundreds of questions that, even with the best preparation, often leaves the test taker discombobulated and anxious. For some would-be physicians, the relentless pressure causes their reasoning abilities to slow or even shut down entirely. The experience—known variously as choking, brain freeze, nerves, jitters, folding, blanking out, the yips or a dozen other descriptive terms—is all too familiar to virtually anyone who has flubbed a speech, bumped up against writer’s block or struggled through a lengthy exam.
For decades scientists thought they understood what happens in the brain during testing or a battlefront firefight. In recent years a different line of research has put the physiology of stress in an entirely new perspective. The response to stress is not just a primal reaction affecting parts of the brain that are common to a wide array of species ranging from salamanders to humans. Stress, in fact, can cripple our most advanced mental faculties, the areas of the brain most developed in primates.
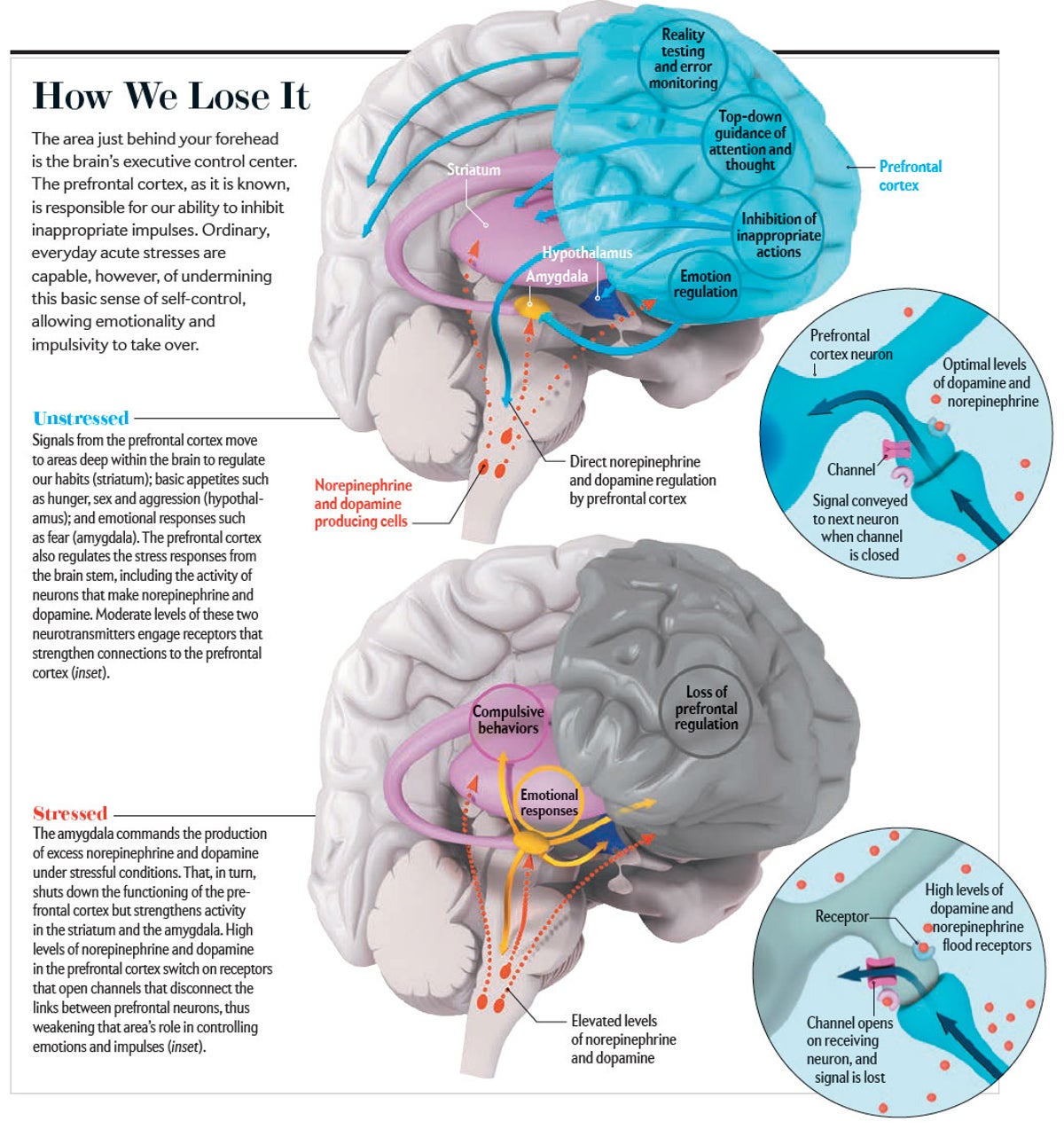
Older textbooks explained that the hypothalamus, an evolutionarily ancient structure lodged at the base of the brain, reacts to stress by triggering the secretion of a wave of hormones from the pituitary and adrenal glands, which makes the heart race, elevates blood pressure and diminishes appetite. Now research reveals an unexpected role for the prefrontal cortex, the area immediately behind the forehead that serves as the control center that mediates our highest cognitive abilities—among them concentration, planning, decision-making, insight, judgment and the ability to retrieve memories. The prefrontal cortex is the part of the brain that evolved most recently, and it can be exquisitely sensitive to even temporary everyday anxieties and worries.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
When things are going well, the prefrontal cortex acts as a control center that keeps our baser emotions and impulses in check. The new research demonstrates that acute, uncontrollable stress sets off a series of chemical events that weaken the influence of the prefrontal cortex while strengthening the dominance of older parts of the brain. In essence, it transfers high-level control over thought and emotion from the prefrontal cortex to the hypothalamus and other earlier-evolved structures. As the older parts take over, we may find ourselves either consumed by paralyzing anxiety or subject to impulses that we usually manage to keep in check: indulgence in excesses of food, drink, drugs or a spending spree at a local specialty store. Quite simply, we lose it.
The growing understanding that acute stress can severely compromise the function of higher “executive” areas in the human brain has drawn the interest of investigators. They are now not just trying to understand what happens in your head when you freeze but also developing behavioral and pharmaceutical interventions to help you keep your composure.
Mind the Jitters
Why we lose it has fascinated scientists for decades. After World War II, investigators analyzed why pilots who were highly skilled in peacetime made simple but fatal mistakes in maneuvering their craft during the heat of battle. What actually happens behind the human skull’s frontal bone remained a mystery until the relatively recent arrival of neuroimaging techniques. In a brain scanner, the riot of activity in the prefrontal cortex gives a clue to just how vulnerable the brain’s master controller is.
The prefrontal cortex is so sensitive to stress because of its special status within the hierarchy of brain structures. It is the most highly evolved brain region, bigger proportionally in humans than in other primates, and makes up a full third of the human cortex. It matures more slowly than any other brain area and reaches full maturity only after the teen years have passed. The prefrontal area houses the neural circuitry for abstract thought and allows us to concentrate and stay on task, while storing information in the mental sketch pad of working memory. This temporary memory storage area operates by allowing us to keep “in mind” such information as the sum of digits that need to be carried over to the next column when performing addition. As a mental-control unit, the prefrontal area also inhibits inappropriate thoughts and actions.
Credit: AXS Biomedical Animation Studio; Source: "Stress Signalling Pathways that Impair Prefrontal Cortex Structure and Function," by Amy F. T. Arnsten, in Nature Reviews Neuroscience, Vol. 10; June 2009
The neurological executive center functions through an extensive internal network of connections among the triangular-shaped neurons called pyramidal cells. These neurons also send out connections to more distant reaches of the brain that control our emotions, desires and habits. When unstressed, the circuits in this network hum along contentedly. Working memory reminds us to start that assignment due next week, and other circuitry sends a message to lower brain regions signaling that it is perhaps best to forgo a second glass of wine. Meanwhile a message to the amygdala, a deep-brain structure that controls fear reactions, provides assurance that the huge hulk approaching on the sidewalk is not about to smash you in the face.
Keeping this network firing as it should can be a fragile process—and when stress hits, even small changes in the neurochemical environment can instantly weaken network connections. In response to stress, our brain floods with arousal chemicals such as norepinephrine and dopamine, which are released by neurons in the brain stem that send projections throughout the brain. Elevated levels of these signaling chemicals in the prefrontal cortex shut off neuron firing, in part by weakening the connection points, or synapses, between neurons temporarily. Network activity diminishes, as does the ability to regulate behavior. These effects only worsen as the adrenal glands near the kidneys, on command from the hypothalamus, spritz the stress hormone cortisol into the bloodstream, sending it to the brain. In this circumstance, self-control depends on a tricky balancing act.
“Keeping one’s cool” is an expression that accurately represents the underlying biological processes. The neural machinery of the prefrontal cortex—and its ability to muster working memory to stay focused on the task at hand—may keep the cascade of neurotransmitters generated deep within the brain from triggering a panicked tide of emotion.
Our research clarifying how easily the prefrontal cortex can be shut down started about 30 years ago. Studies in animals by one of us (Arnsten), along with the late Patricia Goldman-Rakic of Yale University, were among the first to illustrate how neurochemical changes during stress can rapidly switch off prefrontal function. The work showed that neurons in the prefrontal cortex disconnect and stop firing after being exposed to a flood of neurotransmitters or stress hormones.
In contrast, areas deep within the brain take a stronger hold over our behavior. Dopamine arrives at a series of deep-brain structures, collectively called the basal ganglia, that regulate cravings and habitual emotional and motor responses. The basal ganglia hold sway not only when we ride a bicycle without falling but also when we indulge in addictive habits, such as those that make us long for that forbidden ice cream.
In 2001 Benno Roozendaal, now at Radboud University in the Netherlands, James McGaugh of the University of California, Irvine, and their colleagues found similar changes in the amygdala, another older brain region. In the presence of norepinephrine and cortisol, the amygdala alerts the rest of the nervous system to prepare for danger and also strengthens memories that are related to fear and other emotions.
This research now extends to humans. These studies have begun to show that some people seem more vulnerable than others because of their genetic makeup or because of a previous history of stress exposure. After dopamine and norepinephrine switch off circuits in the prefrontal area required for higher cognition, enzymes normally chew up the neurotransmitters so that the shutdown does not persist. In this way, we can return to our baseline when stress abates. Certain forms of a gene can weaken these enzymes, making people more vulnerable to stress and, in some cases, mental illness. Similarly, environmental factors can increase vulnerability; for example, lead poisoning can mimic aspects of the stress response and erode cognition.
Still other research focuses on what happens when the assault on the prefrontal cortex lasts for days or weeks. Chronic stress appears to expand the intricate web of connections among neurons in our lower emotional centers, whereas the areas engaged during flexible, sustained reasoning—anything from the philosophy of Immanuel Kant to calculus—start to shrivel. Under these conditions, the branching, signal-receiving dendrites in the primal amygdala enlarge, and those in the prefrontal cortex shrink. John Morrison of the Icahn School of Medicine at Mount Sinai and his colleagues have shown that prefrontal dendrites can regrow if the stress disappears, but this ability to rebound may vanish if the stress is especially severe. One of us (Sinha) has found evidence of this in humans, where the shrinkage in prefrontal gray matter relates to the history of stress exposure.
This chain of molecular events makes us more vulnerable to subsequent stress and most likely contributes to depression, addiction and anxiety disorders, including post-traumatic stress. Gender appears to be a factor in determining how we react to stress. In women, the hormone estrogen may amplify sensitivity. For example, as one of us (Mazure) and her colleagues have shown, life stress poses a greater risk for depression and is more likely to reduce abstinence from certain addictive behaviors, such as smoking, in women as compared with men. In men, stress may play a more prominent role in exacerbating cravings and eliciting habitual behaviors mediated by the basal ganglia. Reactions that are linked to a specific life stressor are set in a psychosocial context that also can be different for women and men. In ongoing research on frontline health-care workers confronting health risks associated with the COVID-19 pandemic, Mazure and her colleagues are finding that women may have higher rates of stress-related symptoms in response to this experience, and they also have higher rates of concurrent “background stress” such as family or caregiving responsibilities and lower income. This suggests that, for women, biological systems may be chronically on alert, thus presenting an increased challenge in negotiating a significant life stress.
More work on how stress alters the brain’s prefrontal self-control locus remains to be done. Some researchers are investigating how other neurochemicals affect the prefrontal cortex. Trevor W. Robbins and Angela Roberts, both at the University of Cambridge, are looking at whether serotonin, which plays a key role in depression, may modulate stress and anxiety through its actions in the prefrontal cortex.

Credit: Dan Saelinger
These studies remain challenging because modern ethical standards for experiments using humans state that subjects should not be exposed to situations of extreme psychological stress, and indeed human study participants are told they can stop at any time, giving them control over the experimental situation in a manner that does not mimic real-life stress. Several laboratories have succeeded in simulating the effects of uncontrolled stress by having study participants watch disturbing movies or, as done by the Sinha group, briefly imagine their own stressful experiences to tap into their reactions.
One question that still perplexes researchers is why the brain has built-in mechanisms to weaken its highest cognitive functions. We still do not know for sure, but the triggering of these primal reactions may perhaps have saved human lives when a predatory wild animal was lurking in the bushes. If we suddenly see a tiger burning bright in the forest, it is far more useful to freeze so that the animal cannot see us than to be remembering the words of William Blake’s poem.
Absent our slow, deliberate higher-brain networks, primitive brain pathways can stop us on a dime or ready us to flee. These mechanisms may serve a similar function when we face danger in the modern world—say, when a reckless driver cuts us off and we need to slam on the brakes. If we remain in this state, though, prefrontal function weakens, a devastating handicap in circumstances where we need to engage in complex decision-making about a loved one’s serious medical condition or organize an important project on a tight deadline.
Get Ahold of Yourself
A logical response to our growing understanding of the jitters is to devise strategies to keep our neural-control center intact. Scientists hope that understanding the molecular events that cause the brain to degenerate from a “reflective” to a “reflexive” state may lead to better treatments for stress disorders. Some of these insights confirm what we already know. Training for emergencies or for military service is all about teaching the basal ganglia and other brain structures to learn the automatic reactions needed to survive. Animal research suggests that the sense of psychological control that becomes second nature to a soldier or emergency medical technician remains the deciding factor in whether we fall apart during stress. Public speaking exhilarates those who feel confident before an audience. For others, it induces nothing but terror, and their minds “go blank.”
The routines of the drill sergeant are mirrored by animal studies that show that juveniles grow up to be more capable in handling stress if they have had multiple, successful experiences confronting mild stress in their youth. Similarly, human studies indicate that success in managing challenging situations can build resilience. In contrast, if children stumble through these experiences, they can become more sensitive to and burdened by stress and depression when they grow up.
Clues to new treatments may be slowly emerging from the lab. The drug prazosin, a generic therapy for blood pressure that blocks some of norepinephrine’s detrimental actions, appears to decrease both alcohol cravings and levels of consumption. In 2011 Sherry McKee of Yale and her colleagues found that another generic medication for blood pressure, called guanfacine, can inhibit some stress reactions and strengthen prefrontal cortical networks, helping people to resist smoking during stress exposure. (Arnsten and Yale University received royalties from Shire Pharmaceuticals for an extended-release form of guanfacine used for treatment of attention-deficit hyperactivity disorder for children and adolescents but did not receive royalties for the immediate-release form of the drug used in adults in this study.) Further, many labs have shown that behavioral strategies such as relaxation, deep breathing and meditation can reduce the stress response.
And what about that sense of control? Perhaps by learning about how the brain reacts to stress, you may come away with an enhanced sense of control. So maybe the next time you are taking a test or speaking in public and your mind goes blank, you can say to yourself, “This is just my brain trying to save me from a tiger.” Maybe it will bring a comforting smile to your face even if it does not bring the correct answer or word to mind.
