Abstract
Purpose
Metastatic spinal cord compression (MSCC) requires expeditious treatment. While there is no ambiguity in the literature about the urgency of care for patients with MSCC, the effect of timing of surgical intervention has not been investigated in detail. The objective of our study was to investigate whether or not the ‘timing of surgery’ is an important factor in survival and neurological outcome in patients with MSCC.
Methods
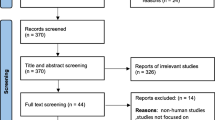
All patients with MSCC presenting to our unit from October 2005 to March 2010 were included in this study. Patients were divided into three groups—those who underwent surgery within 24 h (Group 1, n = 45), between 24 and 48 h (Group 2, n = 23) and after 48 h (Group 3, n = 53) from acute presentation of neurological symptoms. The outcome measures studied were neurological outcome (change in Frankel grade post-operatively), survival (survival rate and median survival in days), incidence of infection, length of stay and complications.
Results
Patients’ age, gender, revised Tokuhashi score, level of spinal metastasis and primary tumour type were not significantly different between the three groups. Greatest improvement in neurology was observed in Group 1, although not significantly when compared against Group 2 (24–48 h; (p = 0.09). When comparisons of neurological outcome were performed for all patients having surgery within 48 h (Groups 1 and 2) versus after 48 h (Group 3), the Frankel grade improvement was significant (p = 0.048) favouring surgery within 48 h of presentation. There was a negative correlation (−0.17) between the delay in surgery and the immediate neurological improvement, suggesting less improvement in those who had delayed surgery. There was no difference in length of hospital stay, incidence of infection, post-operative complications or survival between the groups.
Conclusions
Our results show that surgery should be performed sooner rather than later. Furthermore, earlier surgical treatment within 48 h in patients with MSCC resulted in significantly better neurological outcome. However, the timing of surgery did not influence length of hospital stay, complication rate or patient survival.

Similar content being viewed by others
References
Byrne TN (1992) Spinal cord compression from epidural metastases. N Engl J Med 327(9):614–619
Nelson KA, Walsh D, Abdullah O, McDonnell F, Homsi J, Komurcu S et al (2000) Common complications of advanced cancer. Semin Oncol 27(1):34–44
Bucholtz JD (1999) Metastatic epidural spinal cord compression. Semin Oncol Nurs 15(3):150–159
McLinton A, Hutchison C (2006) Malignant spinal cord compression: a retrospective audit of clinical practice at a UK regional cancer centre. Br J Cancer 94(4):486–491
Constans JP, de Divitiis E, Donzelli R, Spaziante R, Meder JF, Haye C (1983) Spinal metastases with neurological manifestations. Review of 600 cases. J Neurosurg 59(1):111–118
Gilbert RW, Kim JH, Posner JB (1978) Epidural spinal cord compression from metastatic tumor: diagnosis and treatment. Ann Neurol 3(1):40–51
Findlay GF (1984) Adverse effects of the management of malignant spinal cord compression. J Neurol Neurosurg Psychiatry 47(8):761–768
Sorensen S, Borgesen SE, Rohde K, Rasmusson B, Bach F, Boge-Rasmussen T et al (1990) Metastatic epidural spinal cord compression. Results of treatment and survival. Cancer 65(7):1502–1508
Sundaresan N, Sachdev VP, Holland JF, Moore F, Sung M, Paciucci PA et al (1995) Surgical treatment of spinal cord compression from epidural metastasis. J Clin Oncol 13(9):2330–2335
Harrington KD (1997) Orthopedic surgical management of skeletal complications of malignancy. Cancer 80(8 Suppl):1614–1627
Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ et al (2005) Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 366(9486):643–648
Furstenberg CH, Wiedenhofer B, Gerner HJ, Putz C (2009) The effect of early surgical treatment on recovery in patients with metastatic compression of the spinal cord. J Bone Jt Surg Br 91(2):240–244
Chaichana KL, Woodworth GF, Sciubba DM, McGirt MJ, Witham TJ, Bydon A et al (2008) Predictors of ambulatory function after decompressive surgery for metastatic epidural spinal cord compression. Neurosurgery 62(3):683–692 (discussion 83–92)
Metastatic Spinal Cord Compression. Diagnosis and management of patients at risk of or with metastatic spinal cord compression (November 2008). Developed for NICE by the National Collaborating Centre for Cancer (CG75). http://www.nice.org.uk/nicemedia/pdf/CG75NICEguideline.pdf
Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J (2005) A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976) 30:2186–2191
Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH et al (1969) The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia 7(3):179–192
Wise JJ, Fischgrund JS, Herkowitz HN, Montgomery D, Kurz LT (1999) Complication, survival rates, and risk factors of surgery for metastatic disease of the spine. Spine (Phila Pa 1976) 24(18):1943–1951
Tancioni F, Navarria P, Pessina F, Attuati L, Mancosu P, Alloisio M, Scorsetti M, Santoro A, Baena RR (2012) Assessment of prognostic factors in patients with metastatic epidural spinal cord compression (MESCC) from solid tumor after surgery plus radiotherapy: a single institution experience. Eur Spine J 21(Suppl 1):S146–S148
Li H, Gasbarrini A, Cappuccio M, Terzi S, Paderni S, Mirabile L, Boriani S (2009) Outcome of excisional surgeries for the patients with spinal metastases. Eur Spine J 18(10):1423–1430
Acknowledgments
The authors would like to thank Dr Graham Warren, Research Fellow in Medical Statistics, Nottingham Integrated Clinical Research Centre, Queen’s Medical Centre, Nottingham for statistical support.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Quraishi, N.A., Rajagopal, T.S., Manoharan, S.R. et al. Effect of timing of surgery on neurological outcome and survival in metastatic spinal cord compression. Eur Spine J 22, 1383–1388 (2013). https://doi.org/10.1007/s00586-012-2635-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2635-y